Addiction is a Habit
 For decades, addiction was viewed as a moral failing—a conscious choice made by individuals who lacked willpower. However, advances in neuroscience have reshaped our understanding, revealing that addiction is far less about deliberate choice and far more about deeply ingrained habits shaped by the brain’s learning and reward systems. Evidence from brain imaging, behavioral studies, and neurobiology shows that addiction reflects the hijacking of habit circuits rather than the exercise of free will.
For decades, addiction was viewed as a moral failing—a conscious choice made by individuals who lacked willpower. However, advances in neuroscience have reshaped our understanding, revealing that addiction is far less about deliberate choice and far more about deeply ingrained habits shaped by the brain’s learning and reward systems. Evidence from brain imaging, behavioral studies, and neurobiology shows that addiction reflects the hijacking of habit circuits rather than the exercise of free will.
The Brain’s Reward System and Habit Formation
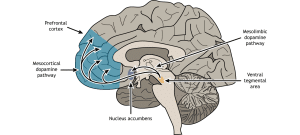
At the center of this discussion is the brain’s reward pathway, primarily involving the mesolimbic dopamine system. Drugs, alcohol, and even compulsive behaviors such as gambling or social media use flood the brain with dopamine. This neurotransmitter signals reward and reinforces behaviors that are repeated. Normally, this system helps us learn adaptive habits, like eating or exercising. But with addictive substances or behaviors, the dopamine surge is far stronger than natural rewards, producing an artificial reinforcement loop.
Over time, repeated use transitions from voluntary experimentation into compulsive habit. Neuroscience research shows that the striatum—a brain region responsible for habit learning—becomes increasingly engaged. Early drug use is associated with the ventral striatum (linked to pleasure), but as addiction develops, control shifts to the dorsal striatum, which governs automatic, habitual behaviors. This shift explains why people continue to seek substances long after the pleasure fades: the brain has encoded the act as a habit, no longer dependent on conscious decision-making.
Prefrontal Cortex and Impaired Choice
Another key piece of evidence lies in the functioning of the prefrontal cortex, the brain’s executive center. This region governs self-control, long-term planning, and decision-making. Chronic drug exposure weakens prefrontal activity, reducing an individual’s capacity to weigh consequences or inhibit impulses. Functional MRI studies show diminished connectivity between the prefrontal cortex and reward centers in addicted individuals, meaning the very brain networks needed to make “choices” are compromised. In this light, addiction cannot be reduced to conscious decision; the machinery of decision-making itself is altered.
Habit Loops and Craving
Habits rely on cue-routine-reward loops, and addiction intensifies these circuits. Environmental triggers such as a bar, a stressful event, or even a certain time of day can unconsciously activate cravings. The hippocampus and amygdala store strong associative memories between cues and drug use, making relapse more likely even after long abstinence. Neuroscientific studies demonstrate that these conditioned responses activate before a person is even aware of craving—another indication that addiction operates beneath conscious control.
Neuroscience has made it clear that addiction is not a simple choice, but the result of entrenched habit loops reinforced by dopamine, weakened executive control, and powerful associative memory. This understanding shifts the narrative from blame to treatment. If addiction is a brain-based habit rather than a willful moral failing, then compassion, behavioral therapy, and medical interventions are essential in helping individuals regain control. By reframing addiction as a habit-driven disorder, neuroscience provides both proof and hope: proof that the cycle is not simply a matter of choice, and hope that with treatment, the brain can rewire itself toward recovery.
Willpower and The Habit of Addiction: Why Determination Alone Isn’t Enough
Willpower is often described as the mental strength to resist short-term temptations in order to achieve long-term goals. It is the conscious effort we use to delay gratification, make disciplined choices, and stay aligned with our values. In many areas of life—dieting, studying, or saving money—willpower plays a central role in guiding behavior. However, when it comes to addiction, neuroscience shows that willpower alone is insufficient to break free from the cycle.
Cravings, environmental cues, and stressors further overwhelm the individual’s conscious resolve. Studies demonstrate that exposure to drug-related cues activates the brain’s reward pathways before a person is even aware of craving. This automatic activation leaves little room for rational thought or the application of willpower.
While willpower may help in brief moments, it cannot override the deeply ingrained neurological changes that sustain addiction. True recovery requires more than determination—it demands treatment that rewires the brain through therapy, medical support, and the development of healthier habits. By understanding the limits of willpower, we shift from blaming individuals to providing the comprehensive care necessary for lasting change.
Addiction Is a Habit: How to Reprogram the Brain and Break Free from the Reward Cycle
The Habitual Nature of Addiction
Habits form through a cue-routine-reward cycle. For example, stress (cue) might lead to drinking (routine), which produces temporary relief (reward). Over time, this loop becomes automatic. Addiction magnifies this cycle because substances artificially stimulate dopamine release, strengthening the routine until it overrides rational decision-making. Eventually, the brain’s reward system no longer functions normally, prioritizing the addictive behavior above all else.
Reprogramming the Brain: Neuroplasticity in Action
Fortunately, the brain is adaptable. Neuroplasticity—the ability of neural circuits to change with new experiences—offers hope for recovery. Reprogramming the brain involves disrupting old habit loops and replacing them with new, healthier ones. This process takes time, consistency, and support, but research shows that new neural pathways can override old ones when reinforced repeatedly.
Strategies for Rewiring Reward Loops Once Addiction is a Habit
- Identify Triggers: The first step is recognizing cues that spark cravings—stress, certain people, places, or emotions. Awareness allows individuals to interrupt the cycle before the automatic routine begins.
- Replace, Don’t Just Remove: The brain craves reward. Simply removing the addictive behavior leaves a void. Instead, replacement with healthier routines—exercise, meditation, creative outlets, or social support—provides alternative sources of dopamine reinforcement.
- Strengthen the Prefrontal Cortex: Since addiction weakens self-control circuits, therapies that enhance mindfulness and decision-making are crucial. Cognitive Behavioral Therapy (CBT), mindfulness meditation, and neurofeedback all help restore executive functioning, making it easier to resist destructive habits.
- Gradual, Not Instant, Change: Habits form through repetition, and they break the same way. Recovery is not about one decisive act of will but repeated practice of healthier responses. Each small victory strengthens new neural pathways.
- Social and Environmental Support: Because cues and environments strongly influence behavior, surrounding oneself with supportive people and recovery-oriented settings reduces exposure to triggers. Group therapy and peer accountability further reinforce new behaviors.
- Medical and Therapeutic Interventions: In many cases, medications that reduce cravings or stabilize brain chemistry support the reprogramming process. Combined with therapy, these tools give the brain space to heal and adopt healthier habits.
Addiction is best understood as a powerful habit rooted in the brain’s reward circuitry. Breaking free is not about summoning willpower but about intentionally reprogramming the brain through neuroplasticity. By identifying triggers, replacing destructive routines with healthy ones, strengthening self-control, and seeking social and medical support, individuals can form new patterns that restore balance and purpose. Recovery, then, is not just about abstinence—it is about rewiring the brain to pursue rewards that sustain life rather than destroy it.
Proper Treatment for Addiction to Substances
Addiction to substances such as alcohol, opioids, or stimulants is a complex medical condition that alters brain function, behavior, and overall health. Effective treatment must go beyond detox or abstinence; it requires a comprehensive approach that addresses the physical, psychological, and social dimensions of the disorder. Modern neuroscience and clinical practice show that recovery is possible when treatment is personalized, multi-faceted, and sustained over time.
Medical Stabilization and Detoxification
The first stage of treatment often involves detoxification, the process of safely managing withdrawal symptoms as substances leave the body. Medical supervision during detox is essential, as withdrawal from drugs like alcohol or benzodiazepines can be dangerous. Physicians may prescribe medications such as buprenorphine, methadone, or naltrexone to stabilize brain chemistry and ease cravings. Detox alone, however, is not treatment; it prepares the individual for long-term recovery work.
Inpatient Treatment and Behavioral Therapies
Once stabilized, patients benefit from inpatient treatment and evidence-based behavioral therapies that address the psychological aspects of addiction. Cognitive Behavioral Therapy (CBT) helps individuals identify triggers, challenge distorted thinking, and develop healthier coping strategies. Contingency management uses positive reinforcement to encourage abstinence, while Motivational Interviewing strengthens the patient’s internal drive to change. Group therapy and peer support foster accountability and reduce isolation, reinforcing the idea that recovery is a shared journey.
Addressing Co-Occurring Disorders
Many people with substance use disorders also struggle with depression, anxiety, or trauma. Effective treatment integrates dual-diagnosis care, ensuring that mental health conditions are treated alongside addiction. This prevents relapse by addressing root causes that may fuel substance use.
Long-Term Support and Relapse Prevention
Addiction is a chronic condition, meaning treatment must extend beyond the initial phase. Relapse prevention strategies are crucial, focusing on identifying triggers, developing coping mechanisms, and building resilience. Support groups such as Narcotics Anonymous or SMART Recovery provide ongoing peer reinforcement, while family therapy helps repair strained relationships and builds a healthier support network.
Holistic and Lifestyle Approaches
Healing extends beyond abstinence. Exercise, mindfulness, and nutrition all play roles in restoring balance to the brain and body. Mindfulness meditation, for example, has been shown to strengthen the prefrontal cortex and reduce stress reactivity, making it easier to resist cravings. Occupational therapy and vocational training also support recovery by giving individuals purpose and stability.
Continuity of Care
Proper treatment recognizes that recovery is not linear. A continuum of care—ranging from inpatient rehabilitation to outpatient therapy, sober living homes, and aftercare programs—offers ongoing support at different stages. Each step reinforces progress and reduces the risk of relapse.
Substance addiction rewires the brain and disrupts life at every level, but it is treatable. Proper treatment requires a combination of medical management, behavioral therapy, mental health support, and long-term lifestyle changes. By addressing both the neurological and social aspects of addiction, treatment provides not just sobriety but the foundation for a healthier, more fulfilling life.
How Ambrosia Behavioral Health Treats People with the Habit of Addiction

Medical Support and Stabilization
The journey often starts with medical stabilization. For many, withdrawal symptoms can be overwhelming and even dangerous. Ambrosia’s medical team provides supervised detox services, ensuring safety and comfort during this critical first step. Medications may be used to ease cravings and regulate brain chemistry, allowing patients to enter treatment with clarity and stability.
Behavioral Therapies to Rewire Habits
Since addiction thrives on habit loops, Ambrosia emphasizes therapies that help patients recognize triggers and replace destructive routines with healthier alternatives. Cognitive Behavioral Therapy (CBT) is central, teaching individuals to identify negative thought patterns and respond in new, constructive ways. Motivational Interviewing helps patients strengthen their commitment to change, while group therapy provides accountability and peer connection—crucial elements in breaking the cycle of isolation that addiction fosters. Additionally, treatments like Brain Mapping and Neurofeedback allow Ambrosia’s treatment team to identify areas of the brain most impacted by addiction for each individual and provide stimulus and pharmacological support to help restore neural pathways.
Dual Diagnosis and Mental Health Care
Addiction rarely exists in isolation. Many patients struggle with depression, anxiety, trauma, or other mental health conditions. Ambrosia integrates dual-diagnosis treatment to address both substance use and co-occurring disorders simultaneously. By treating the whole person, not just the addiction, the likelihood of lasting recovery is significantly increased.
Holistic Healing and Lifestyle Change
Ambrosia recognizes that recovery is not only about abstinence—it is about building a fulfilling life. Programs incorporate holistic practices such as mindfulness, meditation, fitness, and nutritional counseling. These approaches strengthen the brain’s self-control circuits, reduce stress reactivity, and promote overall well-being. By offering healthier sources of reward and purpose, Ambrosia helps patients establish routines that support long-term sobriety.
Family Involvement and Community Support
Addiction affects more than the individual—it touches families and communities. Ambrosia involves loved ones in the healing process through family therapy and educational programs. This fosters understanding, repairs relationships, and creates a supportive environment that reinforces recovery outside of treatment.
Relapse Prevention and Aftercare
Recognizing that recovery is a lifelong journey, Ambrosia provides robust aftercare and relapse-prevention strategies. Patients are equipped with tools to manage triggers, navigate stress, and maintain new habits. Alumni programs and peer support networks offer ongoing connection and accountability, helping individuals stay grounded long after they leave formal treatment.
In Conclusion
At Ambrosia Behavioral Health, treatment is built on the belief that while addiction is a powerful habit, the brain is capable of change. Through medical stabilization, evidence-based therapies, holistic care, and long-term support, Ambrosia helps individuals not only break free from destructive patterns but also build healthier, more meaningful lives. Recovery is not just about ending substance use—it is about rewiring the brain for hope, resilience, and lasting wellness.
Additional Resources
Home | SAMHSA – Substance Abuse and Mental Health Services Administration
United Way | Supporting Mental Health and Well-Being For All | United Way Worldwide
FAQ Addiction, Habits, and Treatment
Q: Is addiction a conscious choice?
A: No. Neuroscience shows that addiction is a habit formed through the brain’s reward system. Substances overstimulate dopamine pathways, reinforcing automatic routines that override rational decision-making.
Q: How does addiction become a habit?
A: Addiction forms through the cue-routine-reward loop. For example, stress (cue) triggers drug use (routine), which brings relief (reward). Over time, this loop becomes automatic, shifting control from pleasure-driven brain regions to habit-driven circuits.
Q: Why isn’t willpower enough to stop addiction?
A: Willpower depends on the prefrontal cortex, which governs self-control. Addiction weakens this area, making it harder to resist cravings. Environmental triggers activate cravings before conscious thought, overwhelming determination alone.
Q: Can the brain be reprogrammed after addiction?
A: Yes. Through neuroplasticity, the brain can form new pathways. Recovery involves breaking old habit loops, replacing them with healthier routines, and strengthening self-control through consistent practice and therapy.
Q: What strategies help rewire the brain from addiction?
A: Identifying triggers, replacing harmful routines with healthy behaviors, practicing mindfulness, seeking social support, and using therapy or medication all help retrain the brain’s reward system.
Q: What does proper treatment for substance addiction involve?
A: Effective treatment combines medical stabilization, behavioral therapies, dual-diagnosis mental health care, holistic approaches (nutrition, exercise, mindfulness), and long-term aftercare.
Q: Why is dual-diagnosis important?
A: Many people with addiction also experience depression, anxiety, or trauma. Treating both conditions together prevents relapse and supports whole-person recovery.
Q: How does Ambrosia Behavioral Health treat addiction?
A: Ambrosia views addiction as a habit and uses medical detox, behavioral therapies, dual-diagnosis care, holistic practices, and family involvement. They also provide aftercare and relapse-prevention strategies for long-term support.
Q: What role does family play in treatment?
A: Ambrosia includes family therapy and education, helping loved ones understand addiction and build a supportive environment that reinforces recovery.
Q: Is recovery from addiction really possible?
A: Yes. With comprehensive treatment and support, the brain can be rewired, destructive habits can be replaced with healthier ones, and long-term recovery is achievable.