Understanding how alcohol impacts our health is crucial for everyone. By recognizing the effects of alcohol, people can make better choices about their drinking habits. While moderate alcohol intake may have some health benefits, such as potentially reducing the risk of heart disease, excessive or frequent drinking can lead to various negative consequences, such as ulcers.
Thus, staying aware of one’s alcohol consumption and its potential effects on overall health is vital for staying healthy and making responsible decisions, but also finding help for those who need it.
At Ambrosia Behavioral Health located in South Florida, our experienced team is equipped to offer comprehensive assistance and support to individuals struggling with alcohol misuse. Remember, seeking help is a brave and proactive step towards improving your well-being and overcoming any challenges related to alcohol addiction.
What Classifies Excessive Drinking?
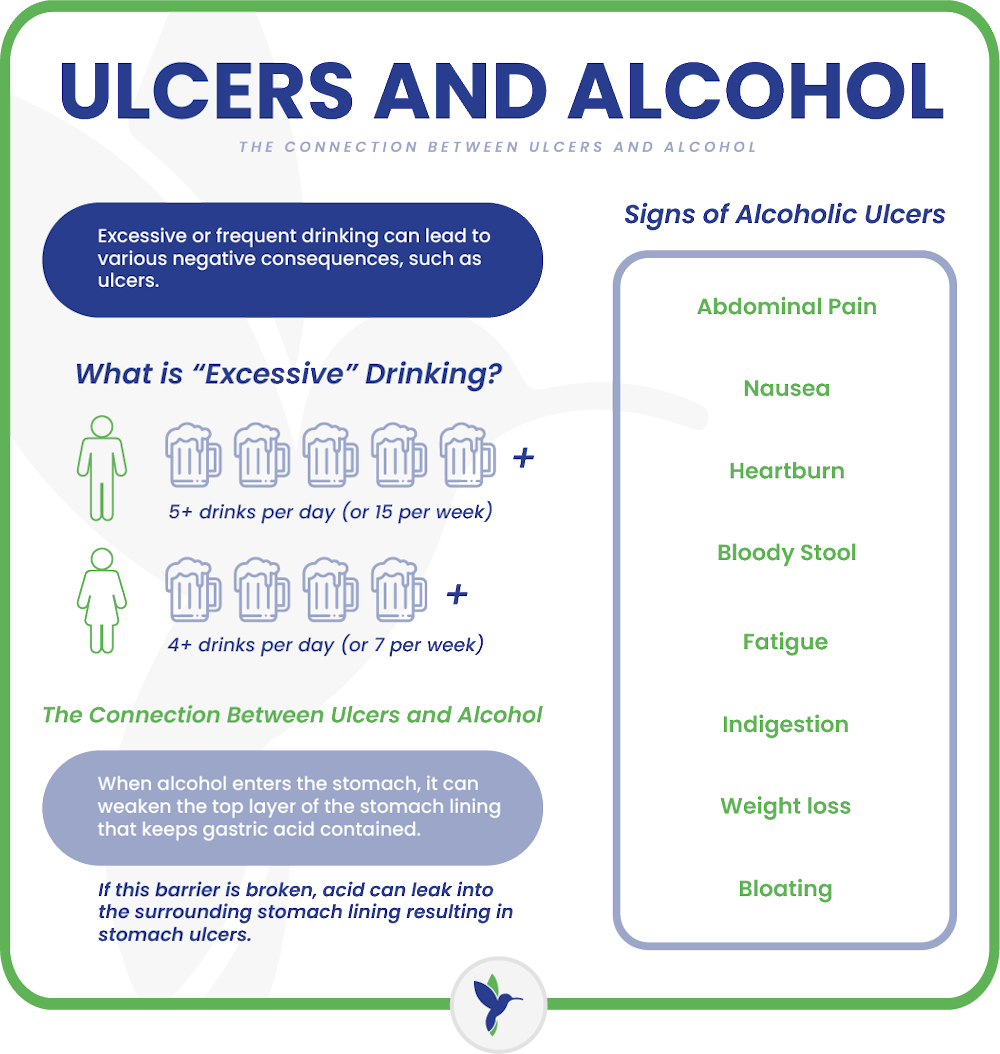 Excessive drinking refers to consuming alcohol in amounts that exceed recommended guidelines or lead to negative consequences for health, safety, or social functioning. It can vary depending on age, gender, weight, and overall health. For most adults, excessive drinking is typically defined as:
Excessive drinking refers to consuming alcohol in amounts that exceed recommended guidelines or lead to negative consequences for health, safety, or social functioning. It can vary depending on age, gender, weight, and overall health. For most adults, excessive drinking is typically defined as:
- For men: Consuming more than 4 drinks on any single day or 14 drinks per week.
- For women: Consuming more than 3 drinks on any single day or 7 drinks per week.
If you find yourself worried about your alcohol consumption, reaching out for help is crucial. One option is to schedule an appointment with your nearby general practitioner (GP) or a specialized drug and alcohol support team.
 Some beverages contain higher alcohol levels than the usual standards. Craft beers, for instance, may have ABV levels exceeding those of regular beers. It is also possible to misjudge the amount of alcohol you are consuming. Large wine glasses, for example, can hold more than five ounces, which is considered one serving of wine. To put it into perspective, a standard wine bottle typically contains about five servings.
Some beverages contain higher alcohol levels than the usual standards. Craft beers, for instance, may have ABV levels exceeding those of regular beers. It is also possible to misjudge the amount of alcohol you are consuming. Large wine glasses, for example, can hold more than five ounces, which is considered one serving of wine. To put it into perspective, a standard wine bottle typically contains about five servings.
To practice moderation effectively, it is crucial to monitor the alcohol content you are consuming in terms of ABV and aim to stay within the lower range of recommendations. Additionally, a useful tip is to consume alcohol with food, particularly fatty foods, as this can slow down its absorption into the bloodstream, ultimately reducing its impact on the body, according to research conducted by Duke University.
Health Problems Linked to Drinking Alcohol
Beyond its effects on the gastrointestinal system, excessive alcohol consumption can also have detrimental impacts on various other parts of the body. Health problems include:
- Mental health: Individuals with alcohol use disorder are more than three times as likely to have experienced major depression in the past year compared to the general population. Alcohol can exacerbate both depression and anxiety by affecting neurotransmitter levels like serotonin.
- Cardiovascular health: Alcohol can elevate cholesterol levels and increase the risk of developing type 2 diabetes, a significant factor in heart disease. Excessive drinking can also raise triglycerides, a type of blood fat that contributes to atherosclerosis.
- Hypertension: While light drinking may not have a significant impact on blood pressure, consuming alcohol in excess can lead to unhealthy increases in blood pressure. This is particularly dangerous for individuals with existing hypertension. Alcohol consumption can indirectly contribute to hypertension by promoting weight gain and increasing the risk of conditions like sleep apnea.
- Cancer risk: Alcohol consumption is associated with a higher risk of various cancers, including breast, colorectal, and liver cancer, as reported by the Centers for Disease Control and Prevention (CDC). Heavy drinking is also linked to an increased risk of stomach and pancreatic cancers. The more alcohol consumed, the greater the risk of developing cancer.
- Liver complications: Excessive alcohol intake can result in the accumulation of fat in the liver, known as fatty liver or hepatic steatosis, as well as inflammation and swelling, referred to as alcoholic hepatitis. These conditions can cause long-term damage to the liver. Some heavy drinkers may develop cirrhosis, which can lead to liver cancer or liver failure.
- Memory problems: Excessive alcohol consumption can lead to memory issues as it temporarily hinders the transfer of memories from short-term to long-term storage in the brain. This can result in alcohol-induced “blackouts” where the individual has no recollection of events that occurred while intoxicated. Furthermore, long-term heavy drinking can cause permanent changes in the brain that impair long-term memory.
- Damage to the pancreas: According to Johns Hopkins Medicine, alcohol abuse is a major contributor to pancreatitis, which is characterized by inflammation in the pancreas. In some cases, this condition can be severe or even life-threatening.
- Weakened immune system: Prolonged heavy drinking weakens the immune system over time, making it more challenging for the body to defend against infections.
Alcohol exerts detrimental effects on various body systems and can have a cascading impact due to sleep disruption and dehydration, both of which are associated with excessive alcohol consumption.
Ulcers and Alcohol: What is the Connection?
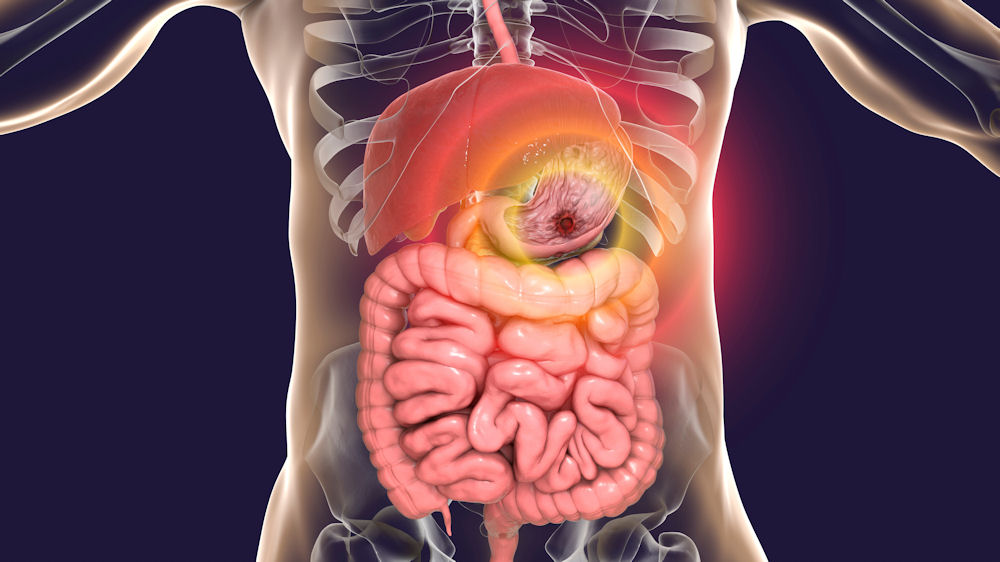
When alcohol enters the stomach, it can weaken something called your gastric mucosal barrier. This is the top layer of the stomach lining that keeps gastric acid—the substance in your stomach responsible for breaking down food—contained so it doesn’t cause damage to stomach tissue. If this barrier is broken, acid can leak into the surrounding stomach lining or into the lining of the upper portion of your small intestine (which sits just below the stomach) and cause it to break or tear. The resulting open sores are called peptic ulcers.
In numerous individuals, peptic ulcers can lead to various complications, even though some individuals may have this condition without experiencing any symptoms. Various factors can heighten the likelihood of developing an ulcer, with alcohol being among them. Understanding the connection and taking steps to safeguard yourself is crucial. Lifestyle choices play a significant role in ulcer prevention or management, with reducing alcohol intake being a key factor.
It is important to note that developing an ulcer due to alcohol consumption is not inevitable; however, regular and excessive alcohol consumption can increase the likelihood of developing one. Additionally, alcohol can impede the healing process of an existing ulcer and potentially worsen the condition.
While alcohol itself doesn’t directly cause ulcers, its effects on stomach acid production, protective mechanisms, inflammation, and healing can contribute to their development and exacerbation. Limiting alcohol intake can help reduce the risk of ulcers and promote better digestive health.
Binge drinking can contribute to the formation of ulcers and alcohol dependency or alcoholism if left untreated. New studies indicate that prolonged, excessive alcohol consumption can contribute to inflammation and various types of harm in the GI tract and digestive system organs, as well as the following:
Alcohol can stimulate the production of stomach acid, which is necessary for digestion but can also irritate the lining of the stomach and intestine. Excessive acid production can erode the protective mucous layer that lines these organs, leading to the formation of ulcers.
Alcohol can weaken the body’s natural defenses against stomach acid. For example, it can inhibit the production of prostaglandins, which help protect the stomach lining from damage. Without enough prostaglandins, the stomach lining becomes more vulnerable to erosion by acid.
Alcohol is a known irritant to the digestive tract. It can directly irritate the lining of the stomach and intestine, leading to inflammation and damage. Chronic inflammation can contribute to the development of ulcers over time.
Helicobacter pylori (H. pylori) is a type of bacteria that is a major cause of peptic ulcers. Alcohol consumption has been linked to an increased risk of H. pylori infection. Once infected, the bacteria can weaken the protective mucous layer and cause inflammation, making the stomach lining more susceptible to ulcer formation.
Chronic alcohol consumption can impair the body’s ability to heal existing ulcers. Alcohol can interfere with the production of new cells and the repair of damaged tissue, prolonging the healing process and increasing the risk of complications.
Chronic alcohol abuse is often associated with inflammation of the stomach lining, a condition known as alcohol-related gastritis or gastropathy. Gastropathy refers to damage to the mucosa, while gastritis involves inflammation of the mucosa. This type of gastritis is frequently linked to an active Helicobacter pylori (H. pylori) infection, a bacterium that can also cause peptic ulcer disease and increase the risk of stomach cancer if left untreated.
These conditions can manifest as either chronic or acute, and abstinence from alcohol can help partially reverse the effects when alcohol is identified as a contributing factor. Excessive alcohol consumption can lead to acute erosive gastropathy, characterized by ulcers, erosions, and bleeding in the stomach lining.
What is An Alcoholic Ulcer?
An alcoholic ulcer occurs when someone drinks too much alcohol over a long time. It’s like a sore that forms in the stomach, intestines, or throat. When alcohol is consumed excessively, it can damage the protective lining of these organs. This damage happens because alcohol increases the production of stomach acid, which can erode the protective layer and lead to ulcer formation. These ulcers can range from small sores to larger wounds, causing discomfort and potentially leading to complications if not addressed.
Recognizing the link between alcohol consumption and the development of peptic ulcers is essential for promoting healthier habits. By being mindful of alcohol intake and seeking support if needed, individuals can reduce the risk of developing alcoholic ulcers and maintain better overall health.
Besides alcohol, there exist two additional substances capable of harming the gastric mucosal barrier: nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin, and a specific bacteria known as helicobacter pylori, or H. pylori. Consequently, consuming alcohol and simultaneously using an NSAID is recognized to elevate the likelihood of experiencing gastrointestinal issues.
Signs and Symptoms of Alcoholic Ulcers
Ulcers caused by excessive alcohol consumption typically manifest with various signs and symptoms. Here are some common ones:
- Abdominal pain: Persistent pain in the upper abdomen, often described as burning or gnawing, is a hallmark of ulcers. It may occur shortly after eating or on an empty stomach.
- Nausea and vomiting: Individuals with alcohol-induced ulcers may experience nausea, sometimes leading to vomiting. Vomiting blood or material that looks like coffee grounds can indicate bleeding ulcers.
- Loss of appetite: A decreased desire to eat can accompany ulcer symptoms, especially if eating worsens the abdominal pain.
- Heartburn: Also known as acid reflux, heartburn is a burning sensation in the chest that may worsen after consuming alcohol or acidic foods.
- Indigestion: Dyspepsia, or indigestion, often occurs alongside ulcers, causing discomfort or a feeling of fullness during or after meals.
- Bloating: Some individuals with ulcers may experience abdominal bloating or a sensation of fullness even without eating much.
- Dark or bloody stools: Ulcers can cause internal bleeding, leading to dark, tarry stools (melena) or stools with visible blood.
- Fatigue: Chronic blood loss from ulcers can lead to iron deficiency anemia, resulting in fatigue, weakness, and pale skin.
- Unexplained weight loss: Severe or persistent ulcers may cause unintended weight loss due to a decreased appetite and difficulty eating.
- Complications: In severe cases, ulcers can lead to complications such as perforation (a hole in the stomach or intestine), obstruction, or severe bleeding, which require immediate medical attention.
It’s important to note that these symptoms can also indicate other gastrointestinal conditions. Therefore, consult a healthcare professional for proper diagnosis and treatment.
Can I Drink Alcohol If I Have A Stomach Ulcer?
If you have a stomach ulcer, it’s generally advisable to avoid drinking alcohol. Alcohol can worsen the symptoms of an ulcer and increase the risk of complications, such as
- Increased pain: Alcohol can further irritate the already sensitive ulcerated tissue, leading to increased pain and discomfort.
- Delayed healing: Alcohol impairs the body’s ability to heal, prolonging the recovery time for ulcers and increasing the risk of complications such as bleeding or perforation.
- Exacerbation of symptoms: Alcohol can exacerbate symptoms such as nausea, vomiting, and heartburn, making the ulcer symptoms more severe and harder to manage.
- Increased risk of bleeding: Alcohol can thin the blood and increase the risk of bleeding from ulcers, which can be life-threatening if not promptly treated.
- Complications: Drinking alcohol with ulcers can increase the risk of developing complications such as gastritis, gastrointestinal bleeding, or perforation, which may require emergency medical attention.
However, individual circumstances may vary, so it’s best to consult with your healthcare provider for personalized advice based on your specific condition and medical history. They can guide whether it’s safe for you to consume alcohol and advise you on any dietary or lifestyle changes that may help manage your ulcer effectively.
Causes and Risk Factors of Alcoholic Ulcers
Several factors contribute to the development of stomach ulcers, and a few are outlined below.
Genetic factors can contribute to a predisposition for developing ulcers by influencing the production and function of proteins involved in maintaining stomach lining integrity and regulating stomach acid secretion. Variations in genes encoding enzymes responsible for acid production or mucosal protective factors can impact susceptibility to ulcers. When combined with heavy alcohol consumption, individuals with such genetic predispositions may face an increased risk and severity of ulcer formation. But genes aren’t the only factor – diet and lifestyle matter too.
Lifestyle factors such as heavy alcohol consumption, smoking, and poor dietary habits can increase the risk of developing ulcers. Excessive alcohol intake can directly irritate the stomach lining and increase stomach acid production, making it more susceptible to damage. Additionally, smoking can weaken the protective mechanisms of the stomach lining, making it more vulnerable to damage from factors such as H. pylori infection or NSAID use.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen, are commonly used to relieve pain and inflammation. However, long-term or excessive use of NSAIDs can irritate the stomach lining and increase the risk of developing ulcers. Alcohol consumption, along with NSAID use, can compound this risk by further irritating the stomach lining and increasing stomach acid production.
Overall, a combination of these factors can contribute to the development of ulcers in individuals who consume alcohol regularly. It’s important to address risk factors with lifestyle changes and, if needed, medical care to effectively prevent or manage ulcers.
Treatment for Ulcers and Alcohol Addiction
 Treating alcoholic ulcers involves tackling both the alcohol abuse and the ulcer itself with a comprehensive approach. This means addressing both the physical and psychological aspects of alcohol abuse. Seeking medical help and following your doctor’s recommendations are crucial for the best outcomes.
Treating alcoholic ulcers involves tackling both the alcohol abuse and the ulcer itself with a comprehensive approach. This means addressing both the physical and psychological aspects of alcohol abuse. Seeking medical help and following your doctor’s recommendations are crucial for the best outcomes.
The first step in treating alcoholic ulcers is to stop drinking alcohol. This helps prevent further damage to the stomach lining and allows the ulcer to heal. To do so, your doctor may prescribe medications to help heal the ulcer and reduce pain. These may include:
- Proton pump inhibitors (PPIs) or H2-receptor antagonists reduce stomach acid production and promote ulcer healing.
- Antacids neutralize stomach acid and relieve pain.
- Antibiotics treat infections; alcohol abuse weakens immunity, heightening the risk of bacterial infections.
In addition to stopping alcohol consumption, making other lifestyle changes can help improve ulcer healing and prevent recurrence. These may include:
- Eating a healthy diet rich in fruits, vegetables, and whole grains.
- Avoid spicy, acidic, or fatty foods that can irritate the stomach lining.
- Managing stress through relaxation techniques or therapy.
- Quitting smoking can delay ulcer healing and increase the risk of complications.
- Support from loved ones or a group aids sobriety, managing emotional hurdles linked to alcohol abuse and its aftermath.
- If you’re struggling with alcohol addiction, seeking professional help from a therapist, counselor, or support group can provide the necessary support and resources to overcome alcohol dependence and prevent future ulcers.
Regularly checking in with your doctor to track ulcer healing progress and adapt treatment accordingly is necessary for optimal recovery. They may recommend additional tests, such as endoscopy, to check the ulcer’s progress and rule out any complications.
Receive Treatment for Alcoholism at Ambrosia Behavioral Health
Exploring the relationship between ulcers and alcohol, as well as other impacts of alcohol on the brain and body is essential. If you or a loved one are struggling with alcoholism, Ambrosia Behavioral Health in West Palm Beach, FL offers a beacon of hope.
Our comprehensive approach to addiction recovery combines evidence-based substance abuse treatments, compassionate care, and personalized support to guide you toward a life of sobriety. Take the first step towards a brighter future today by contacting us. Let us help you reclaim your life and break the cycle of alcohol addiction.




