MAT: Suboxone, Methadone and Vivitrol: Harm Reduction in Florida

Understanding Harm Reduction and Why Suboxone Matters
Harm reduction is a public health approach that focuses on reducing the real-world risks associated with substance use rather than demanding immediate abstinence as the only acceptable outcome. It recognizes that people enter recovery at different stages, with different motivations, medical histories, and life circumstances. Within this framework, medication-assisted treatment has become one of the most effective tools available for addressing opioid use disorder.
Among the available medications, Suboxone has emerged as one of the most widely used and accessible options in modern harm reduction systems. Suboxone plays a critical role in stabilizing individuals, reducing overdose risk, and helping people regain control of daily life while longer-term recovery goals take shape. When used alongside other evidence-based services, Suboxone helps close the dangerous gap between active opioid use and sustained treatment engagement.
Although harm reduction includes many tools such as education, safer-use strategies, and access to medical care, medications like Suboxone, methadone, and Vivitrol provide a powerful biological foundation that supports safer behavior and long-term outcomes.
Why Suboxone Is a Cornerstone of Harm Reduction
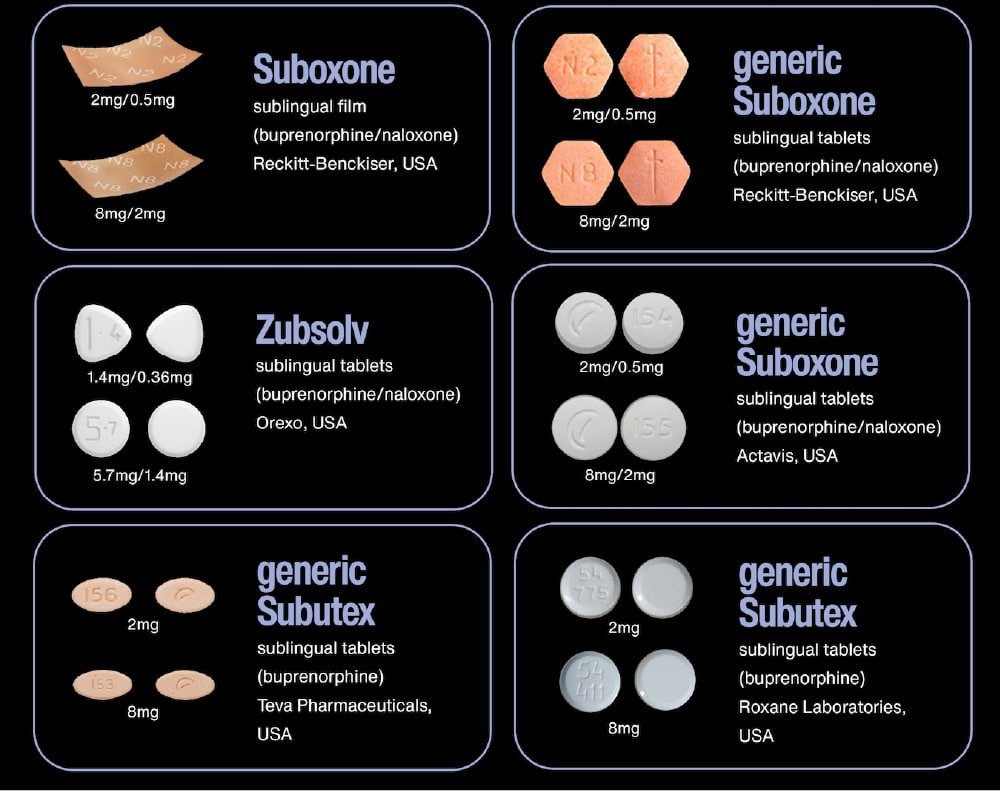
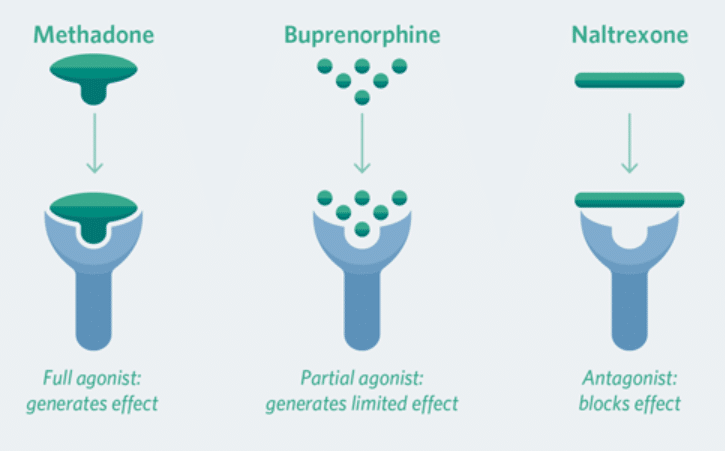
Suboxone is a combination medication containing buprenorphine and naloxone. Buprenorphine is a partial opioid agonist that binds strongly to opioid receptors, easing withdrawal symptoms and cravings without producing the intense euphoria associated with full opioids. Naloxone is included as a misuse deterrent and does not significantly affect the medication when taken as prescribed.
In harm reduction programs, Suboxone is especially valuable because it allows people to stabilize rapidly and safely. Individuals do not need to endure prolonged withdrawal before engaging in care, and they are far less likely to return to high-risk opioid use once Suboxone is properly initiated and monitored.
Suboxone supports harm reduction by dramatically lowering the likelihood of overdose, reducing exposure to contaminated drug supplies, and helping people disengage from unsafe use patterns. For many individuals, Suboxone becomes the bridge that allows them to rebuild relationships, return to work, and participate meaningfully in counseling and recovery services.
Importantly, Suboxone can be prescribed in outpatient medical settings. This accessibility makes Suboxone one of the most scalable and community-friendly options available in harm reduction strategies.
How Suboxone Works in the Body
From a clinical perspective, Suboxone works by occupying opioid receptors in the brain while only partially activating them. This produces enough opioid effect to prevent withdrawal and reduce cravings, but not enough to cause the same respiratory depression and reward response seen with heroin, fentanyl, or prescription opioids.
The high binding affinity of buprenorphine blocks other opioids from attaching to the receptor. As a result, Suboxone acts as a protective barrier against relapse and overdose. Even if someone attempts to use another opioid while stabilized on Suboxone, the euphoric effect is greatly diminished.
Within harm reduction models, this pharmacological profile is crucial. Suboxone allows individuals to reduce or eliminate dangerous opioid use without forcing immediate behavioral perfection. It supports gradual change while improving safety at every stage.
Approaches like naloxone distribution, fentanyl test strips, syringe services, wound care, and peer support lower mortality and improve public health outcomes. They also create consistent points of contact with healthcare systems, making it more likely that individuals will seek medical care, mental health support, and—when ready—treatment and recovery services.
Harm reduction recognizes substance use as a complex health issue, not a moral failing. By prioritizing compassion, safety, and engagement, it builds trust, reduces stigma, and opens the door to long-term recovery and stability for individuals, families, and communities.
Suboxone and Long-Term Engagement in Care
One of the most important benefits of Suboxone is its impact on treatment retention. People who use Suboxone consistently are far more likely to remain engaged in care than those who attempt recovery without medication support.
Harm reduction recognizes that ongoing engagement is more valuable than short-term compliance. Suboxone reduces the physical and psychological barriers that often drive people away from treatment programs. When withdrawal and cravings are controlled, individuals are better able to focus on therapy, housing stability, employment, and mental health care.
Suboxone also reduces the cycle of repeated detox admissions that often place people at heightened risk for overdose after discharge. Stabilization with Suboxone allows recovery planning to happen from a place of safety rather than crisis.
Methadone in Harm Reduction and How It Compares to Suboxone
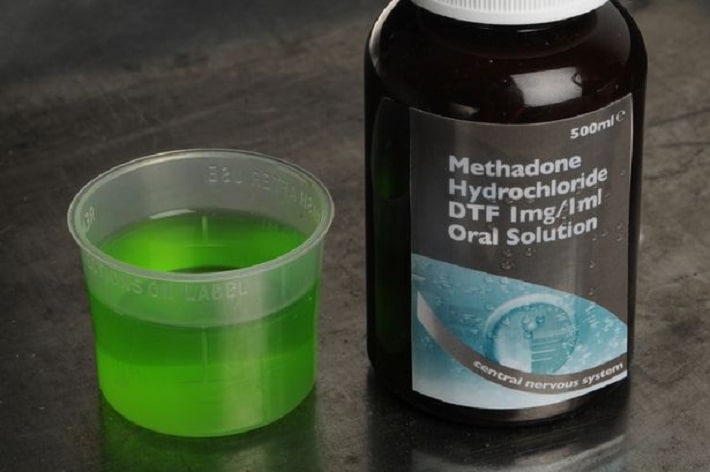
Methadone has been used for decades as a treatment for opioid use disorder and remains an essential part of harm reduction worldwide. Unlike Suboxone, methadone is a full opioid agonist. It activates opioid receptors more fully, which can be beneficial for individuals with very high levels of physical dependence.
Methadone is typically provided through specialized opioid treatment programs with daily supervised dosing, especially during early treatment phases. This structure offers close monitoring and stability for individuals who may struggle with medication adherence or who require higher levels of pharmacological support.
In comparison, Suboxone offers greater flexibility and accessibility. Because Suboxone can be prescribed in office-based settings, people are often able to integrate treatment more easily into daily life. Suboxone’s safety profile also makes it a preferred first-line option in many harm reduction programs, particularly for individuals at elevated risk of respiratory depression or polysubstance use.
Both medications serve harm reduction goals, but Suboxone frequently fits more seamlessly into community-based care models.
When Methadone May Be More Appropriate Than Suboxone
Although Suboxone is effective for many people, there are situations in which methadone may offer better stabilization. Individuals who have repeatedly experienced inadequate symptom control on Suboxone or who require higher levels of opioid receptor activation may respond better to methadone.
Harm reduction emphasizes individualized care. Choosing between methadone and Suboxone is not about hierarchy but about matching the right medication to the right person. For some, methadone provides the structure and pharmacological strength necessary to prevent relapse and overdose.
Still, for many individuals entering harm reduction services for the first time, Suboxone provides a safer and more flexible starting point.
Vivitrol in Harm Reduction and How It Differs from Suboxone
Vivitrol is a long-acting injectable form of naltrexone. Unlike Suboxone and methadone, Vivitrol is not an opioid medication. It is an opioid antagonist that blocks opioid receptors completely.
This difference makes Vivitrol fundamentally distinct in harm reduction practice. Suboxone stabilizes the brain’s opioid system, while Vivitrol shuts it down. To begin Vivitrol safely, individuals must be fully detoxified and free from opioids for a sufficient period of time. Starting Vivitrol too soon can cause severe and sudden withdrawal.
For people who are highly motivated for opioid abstinence and who can complete detoxification safely, Vivitrol may provide strong protection against relapse. However, harm reduction frameworks recognize that requiring full detox before treatment can create barriers and increase overdose risk during the waiting period.
Suboxone, by contrast, can be initiated much earlier and offers immediate relief from withdrawal and cravings. This makes Suboxone more compatible with low-threshold harm reduction programs that prioritize rapid access to care.


Suboxone and Overdose Prevention
One of the most powerful contributions of Suboxone to harm reduction is its effect on overdose prevention. Stabilization on Suboxone significantly reduces illicit opioid use and lowers the likelihood of exposure to unpredictable street drug supplies.
Because Suboxone limits the ability of other opioids to activate receptors, it also provides a protective buffer if relapse occurs. While no medication eliminates risk entirely, Suboxone reduces both the frequency and severity of high-risk opioid use.
In communities heavily impacted by fentanyl and synthetic opioid contamination, Suboxone has become an essential public health tool. It offers a medically supervised alternative to dangerous self-directed attempts to manage withdrawal or reduce use.
Suboxone and Mental Health in Harm Reduction Settings
Opioid use disorder frequently co-occurs with depression, anxiety, trauma, and other psychiatric conditions. Harm reduction recognizes that untreated mental health symptoms often drive relapse and disengagement from care.
Suboxone helps stabilize neurochemical systems that are disrupted by long-term opioid use. As physical dependence becomes manageable, individuals often experience improved emotional regulation and cognitive clarity. This creates a more stable foundation for trauma-informed therapy and psychiatric treatment.
While Suboxone is not a mental health medication, its ability to reduce chronic stress associated with withdrawal and craving supports overall psychological well-being and increases the likelihood that people will continue participating in comprehensive care.
Addressing Stigma Around Suboxone in Harm Reduction
Despite overwhelming evidence supporting medication-assisted treatment, stigma remains a significant barrier. Some people still view Suboxone as simply replacing one drug with another. Harm reduction challenges this narrative by focusing on health outcomes, safety, and quality of life.
Suboxone is a medically prescribed and carefully monitored treatment that reduces mortality, stabilizes brain function, and supports long-term recovery. The goal is not to create dependency but to manage a chronic medical condition with evidence-based tools.
Within harm reduction philosophy, using Suboxone is no different from using insulin to manage diabetes or medication to treat hypertension. It is a practical and compassionate response to a complex medical disorder.
Suboxone in Community-Based Harm Reduction Programs
Suboxone fits naturally into community-based harm reduction initiatives, including mobile clinics, primary care practices, behavioral health centers, and outpatient recovery programs. Low-threshold access to Suboxone allows individuals to receive treatment without excessive administrative barriers or rigid program requirements.
This approach is especially important for people experiencing housing instability, transportation challenges, or inconsistent access to healthcare. Suboxone programs that integrate peer support, counseling, and case management are often able to engage individuals who would otherwise remain disconnected from traditional treatment systems.
By meeting people where they are, Suboxone strengthens the overall harm reduction ecosystem.

Choosing Between Suboxone, Methadone, and Vivitrol
Harm reduction does not promote a single medication as the only valid solution. Instead, it encourages informed decision-making that reflects each person’s medical history, goals, and lived experience.
Suboxone is often the preferred option when rapid access, outpatient flexibility, and a strong safety profile are priorities. Methadone may be more appropriate for individuals with severe dependence or those who benefit from daily clinical structure. Vivitrol may be useful for individuals who have completed detox and prefer a non-opioid medication.
What matters most is that individuals are offered real choices and are supported in finding the medication that best fits their needs.
The Future of Harm Reduction and the Expanding Role of Suboxone
As healthcare systems increasingly adopt harm reduction models, Suboxone continues to play a central role in expanding access to effective treatment. Innovations in telehealth, pharmacy-based services, and integrated primary care are further improving the reach of Suboxone programs.
Research consistently shows that medication-assisted treatment saves lives, reduces healthcare costs, and improves long-term recovery outcomes. Suboxone, in particular, remains one of the most powerful tools for reducing overdose deaths and stabilizing communities affected by the opioid crisis.
Harm reduction is not about lowering expectations. It is about raising standards of care by prioritizing evidence, dignity, and safety. Suboxone represents a practical and compassionate response to opioid use disorder, one that recognizes recovery as a process rather than a single moment of change.
FAQ Section on Methadone, Suboxone and Vivitrol
What is Suboxone and why is Suboxone so important in harm reduction?
Suboxone is a prescription medication used to treat opioid use disorder, and it plays a central role in harm reduction because it lowers overdose risk while stabilizing the brain and body. Suboxone helps control withdrawal symptoms and cravings, which allows people to reduce or stop dangerous opioid use without being forced into immediate abstinence. In harm reduction settings, Suboxone is especially valuable because it can be started quickly, offered in outpatient care, and adapted to each person’s pace of recovery.
Is Suboxone just replacing one drug with another?
This is one of the most common misunderstandings about Suboxone. Suboxone is not intended to create a new addiction. It is a medically supervised treatment that helps regulate opioid receptors in the brain so that cravings, withdrawal, and compulsive use decrease. In harm reduction, Suboxone is viewed as a life-saving medication that treats a chronic medical condition. The goal of Suboxone is stability, safety, and improved quality of life, not intoxication.
How does Suboxone reduce the risk of overdose?
Suboxone lowers overdose risk in several important ways. It reduces the need to use illicit opioids, which often contain unpredictable and dangerous substances such as fentanyl. Suboxone also binds tightly to opioid receptors, making it harder for other opioids to attach and cause respiratory depression. In harm reduction programs, consistent use of Suboxone is strongly associated with fewer overdoses and fewer emergency medical events.
What is the difference between Suboxone and methadone in harm reduction?
Suboxone and methadone are both effective medications for opioid use disorder, but they work differently. Suboxone is a partial opioid agonist and has a strong safety profile, making it well suited for outpatient and community-based harm reduction programs. Methadone is a full opioid agonist and is usually provided through specialized clinics with daily supervision. Suboxone is often chosen when flexibility, access, and lower overdose risk are priorities, while methadone may be better for people with more severe physical dependence.
Can Suboxone be started right away in harm reduction programs?
In many cases, Suboxone can be started relatively quickly compared to other treatment options. This is one of the reasons Suboxone fits so well within harm reduction models. People do not need to complete long detox programs before receiving Suboxone, and access can often occur through primary care or outpatient behavioral health providers. Rapid access to Suboxone helps prevent relapse and overdose during high-risk periods.
How is Vivitrol different from Suboxone in harm reduction?
Vivitrol works very differently from Suboxone. Suboxone stabilizes opioid receptors and reduces withdrawal and cravings. Vivitrol blocks opioid receptors completely and requires that a person be fully detoxified before the first dose. In harm reduction settings, Suboxone is often easier to start and maintain because it does not require extended opioid-free periods. Vivitrol may be helpful for some individuals who have already completed detox and prefer a non-opioid medication, but Suboxone generally offers broader access and lower treatment barriers.
How long do people usually stay on Suboxone in harm reduction care?
There is no single correct length of time for Suboxone treatment. Harm reduction approaches emphasize individualized care, and many people remain on Suboxone for months or years. Some continue Suboxone as long-term maintenance because it supports stability and prevents relapse. Decisions about tapering or continuing Suboxone should be made collaboratively with a medical provider and should be guided by safety, health outcomes, and personal recovery goals.
Does Suboxone help with mental health symptoms?
Suboxone is not a mental health medication, but it often supports emotional and psychological stability indirectly. By reducing withdrawal, cravings, and constant stress related to opioid use, Suboxone creates space for people to engage in therapy and psychiatric care. In harm reduction programs, Suboxone is frequently part of integrated treatment plans that address trauma, depression, anxiety, and other co-occurring conditions.
Does Suboxone help with mental health symptoms?
Suboxone is not a mental health medication, but it often supports emotional and psychological stability indirectly. By reducing withdrawal, cravings, and constant stress related to opioid use, Suboxone creates space for people to engage in therapy and psychiatric care. In harm reduction programs, Suboxone is frequently part of integrated treatment plans that address trauma, depression, anxiety, and other co-occurring conditions.
Can someone still relapse while taking Suboxone?
Relapse can still occur, but Suboxone significantly reduces both the frequency and severity of high-risk opioid use. Suboxone helps protect people during vulnerable moments by lowering cravings and blocking the effects of other opioids. In harm reduction, relapse is treated as a clinical signal rather than a failure, and Suboxone remains a key tool for helping individuals return to stability quickly and safely.




